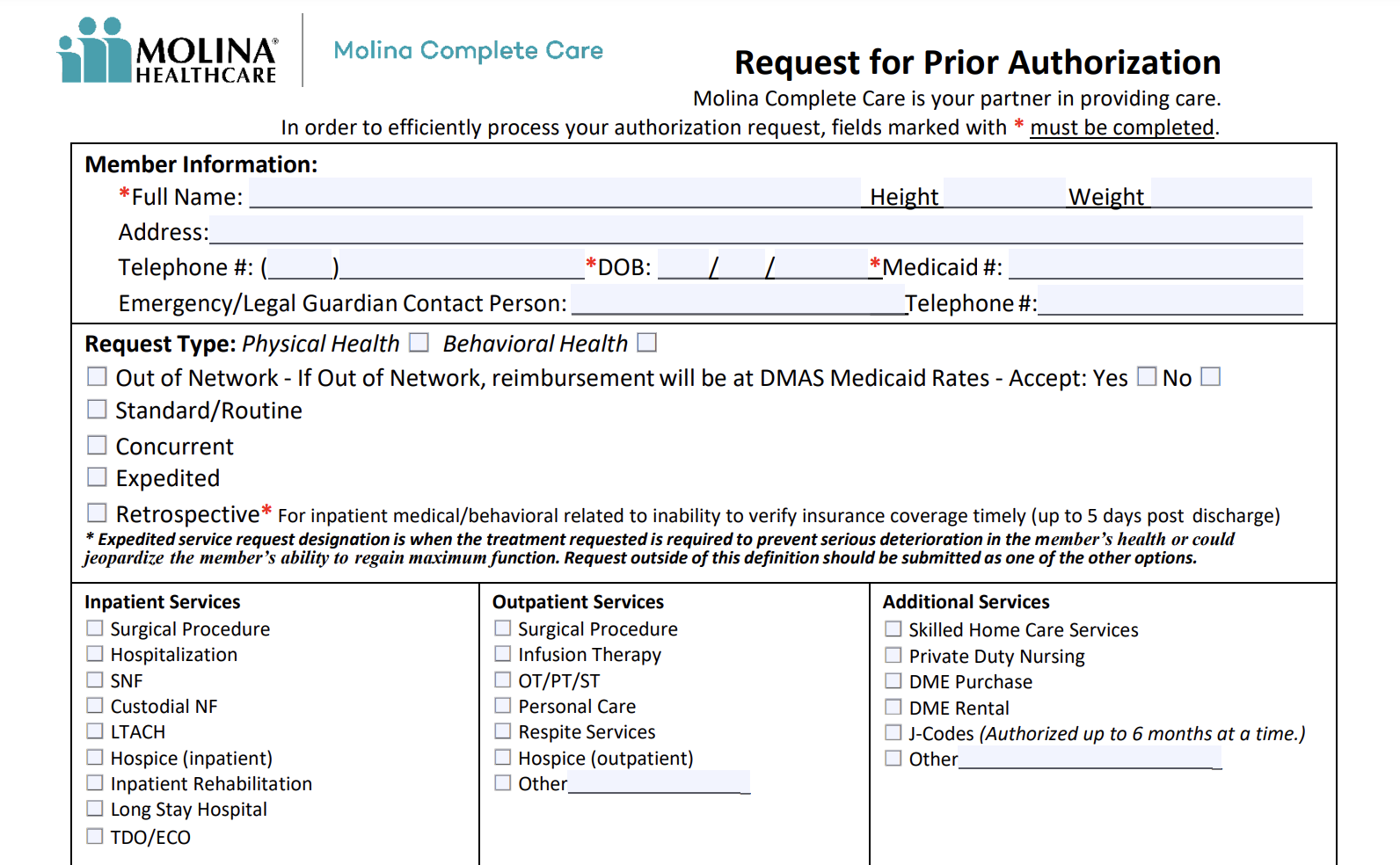
Introducing the Molina Prior Auth Tool, an innovative solution revolutionizing healthcare authorization. This comprehensive tool empowers healthcare providers with unparalleled efficiency and accuracy, transforming the way prior authorizations are processed.
The Molina Prior Auth Tool offers a seamless user experience, ensuring healthcare professionals can navigate the authorization process with ease. Its intuitive interface and step-by-step guidance make it accessible to all, regardless of their technical expertise.
Overview of Molina Prior Auth Tool
The Molina Prior Auth Tool is an online platform that helps healthcare providers request and track prior authorizations for Molina Healthcare members. The tool is designed to streamline the prior authorization process, making it easier for providers to get the approvals they need to provide timely and appropriate care to their patients.
If you’re looking for an easy way to check if your computer is infected with malware, you should try the farbar recovery scan tool. It’s a free and easy-to-use tool that can help you identify and remove malware from your computer.
Once you’ve cleaned your computer of malware, you can use the molina prior auth tool to check for any prior authorizations that may have been made on your account.
The Molina Prior Auth Tool offers a number of benefits to providers, including:
- Faster processing times:The tool automates the prior authorization process, which can significantly reduce processing times.
- Improved accuracy:The tool helps to ensure that prior authorization requests are complete and accurate, which can reduce the risk of denials.
- Increased transparency:The tool provides providers with real-time visibility into the status of their prior authorization requests.
The Molina Prior Auth Tool is also easy to use. Providers can simply create an account and start submitting prior authorization requests online. The tool provides step-by-step instructions and helpful resources to guide providers through the process.
The Molina Prior Auth Tool is a valuable resource for providers who care for Molina Healthcare members. The tool can help providers to improve the efficiency and accuracy of their prior authorization requests, which can lead to better patient care.
How to Use the Molina Prior Auth Tool
The Molina Prior Auth Tool is an online portal that allows providers to submit prior authorization requests to Molina Healthcare. Using the tool is straightforward and can help streamline the prior authorization process.
Step 1: Register for an Account
To use the Molina Prior Auth Tool, you must first register for an account. You can do this by visiting the Molina Healthcare website and clicking on the “Register” link. Once you have registered, you will be able to log in to the tool using your username and password.
Step 2: Submit a Prior Authorization Request
To submit a prior authorization request, log in to the Molina Prior Auth Tool and click on the “Submit a Request” button. You will then be prompted to enter the patient’s information, the procedure or service being requested, and the reason for the request.
You can also upload supporting documentation, such as medical records or test results.
The Molina Prior Authorization Tool is a valuable tool for healthcare providers to streamline the prior authorization process. It can help you save time and improve patient care. If you’re looking for more ways to optimize your practice, consider exploring media planning tools to enhance your patient outreach and engagement strategies.
These tools can help you reach more patients and improve your overall marketing efforts. The Molina Prior Authorization Tool is just one of many tools available to help you improve your practice. By utilizing these resources, you can provide better care for your patients and grow your business.
Step 3: Track the Status of Your Request
Once you have submitted a prior authorization request, you can track its status online. To do this, log in to the Molina Prior Auth Tool and click on the “Track My Requests” button. You will then be able to see the status of all of your pending requests.
Common Challenges and Solutions
- I’m having trouble logging in to the Molina Prior Auth Tool.Make sure that you are using the correct username and password. If you have forgotten your password, you can click on the “Forgot Password” link on the login page.
- I’m not sure how to fill out the prior authorization request form.The Molina Prior Auth Tool provides detailed instructions on how to fill out the request form. You can also contact Molina Healthcare’s customer service department for assistance.
- My prior authorization request was denied.If your prior authorization request is denied, you can appeal the decision. To do this, you will need to submit a written appeal to Molina Healthcare. The appeal should include a detailed explanation of why you believe the decision should be overturned.
Features of the Molina Prior Auth Tool
The Molina Prior Auth Tool offers a suite of features designed to streamline the prior authorization process, enhance efficiency, and improve accuracy. These features empower healthcare providers to navigate the complexities of prior authorization, ensuring timely access to necessary treatments and improved patient outcomes.
Automated Eligibility Verification, Molina prior auth tool
- Verifies patient eligibility for coverage in real-time, eliminating the need for manual checks and reducing processing time.
- Automates the collection of relevant patient information, such as insurance status, coverage details, and benefits, ensuring accurate and complete submissions.
Electronic Prior Authorization Submission
- Allows providers to submit prior authorization requests electronically, eliminating the need for paper-based processes and reducing turnaround time.
- Provides a secure and HIPAA-compliant platform for submitting sensitive patient information, ensuring data privacy and protection.
Real-Time Status Tracking
- Enables providers to track the status of prior authorization requests in real-time, eliminating the need for phone calls or emails to check on progress.
- Provides instant notifications of approval, denial, or additional information requests, allowing for prompt follow-up and resolution.
Integrated Decision Support
- Offers clinical guidance and evidence-based criteria to support decision-making during the prior authorization process.
- Assists providers in determining the appropriate level of care, reducing the risk of denials and improving patient outcomes.
Enhanced Reporting and Analytics
- Provides comprehensive reporting and analytics capabilities to track prior authorization trends, identify areas for improvement, and optimize performance.
- Helps healthcare organizations measure the efficiency and effectiveness of their prior authorization processes, leading to data-driven decision-making.
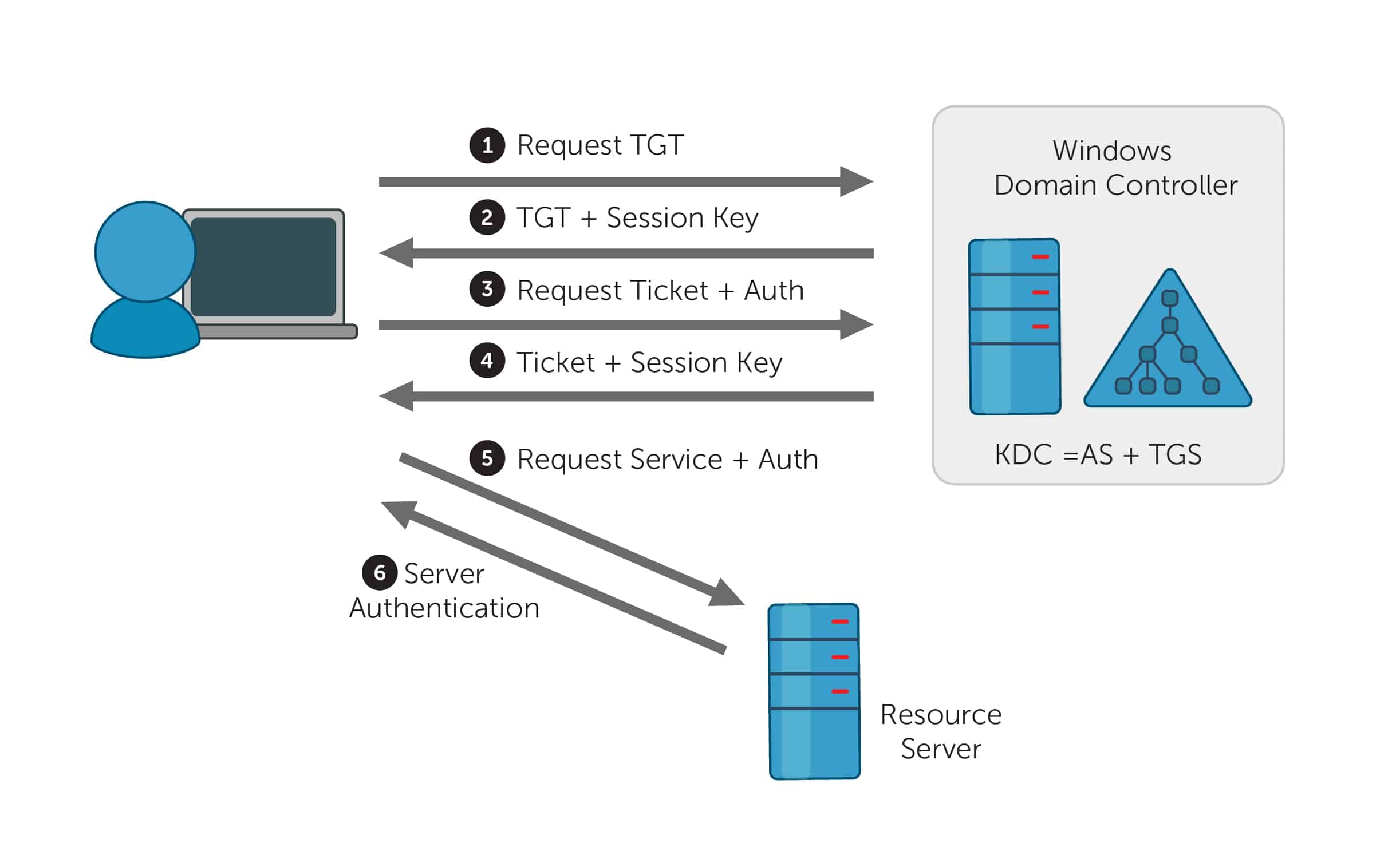
Integration with Other Systems
The Molina Prior Auth Tool seamlessly integrates with various healthcare systems to enhance data sharing and streamline operations.
This integration offers numerous benefits, including:
- Improved data accuracy and consistency
- Reduced duplication of effort and manual processes
- Enhanced patient care coordination
Successful Integrations
The Molina Prior Auth Tool has been successfully integrated with several healthcare systems, including:
- Electronic health records (EHRs)
- Claims processing systems
- Pharmacy management systems
These integrations have resulted in significant improvements in prior authorization processes, leading to faster approvals, reduced costs, and improved patient outcomes.
Best Practices for Using the Molina Prior Auth Tool
To maximize the efficiency and accuracy of the Molina Prior Auth Tool, it’s essential to follow best practices. These practices will help you streamline your workflow, reduce errors, and ensure timely approvals.
To begin with, it’s important to familiarize yourself thoroughly with the tool’s features and functionality. By understanding the capabilities of the tool, you can effectively leverage it to meet your specific needs.
Data Preparation and Organization
Proper data preparation and organization are crucial for efficient prior authorization submissions. Ensure that all necessary patient information, medical records, and supporting documentation are gathered and organized before initiating the submission process. This will save time and prevent delays due to missing or incomplete information.
Clear and Concise Requests
When submitting a prior authorization request, it’s essential to provide clear and concise information. Clearly state the reason for the request, including the specific procedure or medication being requested. Provide detailed medical justification to support your request, ensuring that the reviewer has a comprehensive understanding of the patient’s condition and treatment plan.
Timely Follow-Up
To avoid delays in the approval process, it’s important to follow up on submitted requests promptly. Regularly check the status of your submissions and respond promptly to any requests for additional information or clarification. By staying proactive, you can expedite the approval process and ensure timely access to necessary treatments for your patients.
Collaboration and Communication
Effective communication and collaboration with the Molina Prior Auth team is essential for successful prior authorization outcomes. If you encounter any challenges or have questions during the submission process, do not hesitate to reach out to the team for assistance.
Clear communication will help resolve issues quickly and facilitate a smooth approval process.
FAQ Guide
What are the key benefits of using the Molina Prior Auth Tool?
The Molina Prior Auth Tool offers numerous benefits, including improved efficiency, reduced errors, enhanced compliance, and better patient outcomes.
How does the Molina Prior Auth Tool integrate with other healthcare systems?
The Molina Prior Auth Tool seamlessly integrates with various healthcare systems, including electronic health records (EHRs) and claims processing systems, enabling smooth data exchange and eliminating duplicate data entry.
What are the best practices for using the Molina Prior Auth Tool?
To maximize the effectiveness of the Molina Prior Auth Tool, it is recommended to establish clear workflows, train staff thoroughly, and regularly review and optimize the authorization process.